Documentation is an age-old idea which has existed since the existence of language. One of the use-cases of documentation has been to preserve history. In medical science, one thing common to all treatments is patient history. Patient history ranges from symptoms, diagnosis, intervention, medication and vital parameters etc. With such diverse information, it becomes helpful to have a framework of organising this information. One of the very first attempts to have such a framework was made by Dr. Lawrence Weed in the 1960’s at the University of Vermont.1 This framework was called the Problem-orientated medical record (POMR). Over time, various disciplines adapted this framework to their own specific uses and evolved into modern note-taking frameworks like SOAP notes, DAP notes and BIRP notes.
SOAP documentation format commands a widespread adoption in the field of healthcare across specialities. This clear, concise and well-organised documentation format has become one of the favourite notes frameworks of behavioral health practitioners. Let us deep dive and learn more about this format.

What is a SOAP note?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym represents a cognitive framework to help healthcare professionals organise treatment information of a client in a highly structured format.
SOAP Notes template with example
A SOAP note is structured into four parts;
Subjective
This section focusses on the subjective experience of the patient or their caretaker. It includes the symptoms they are experiencing, feelings w.r.t. the illness, medical history, previous diagnosis (if any), and their personal views. Simply put, this is what the patient says about their problem.
Example: 37-year old female presenting chest pain, decreased appetite and shortness of breath. Diagnosed with mild depression 1 year ago. Underwent psychotherapy for 3 months. Recent physical manifestations concurrent with family feuds.
Objective
The focus of this section is on objective data. This includes vital signs and symptoms, findings of the clinician, laboratory diagnostic data and objective reports from other clinicians. Unlike the “Subjective” section which gives a description of patient’s own account, the “Objective” section is backed by evidence. An example of this is a patient stating they have “stomach pain,” which is documented under the subjective heading. Versus “abdominal tenderness to palpation,” an objective sign documented under the objective heading.
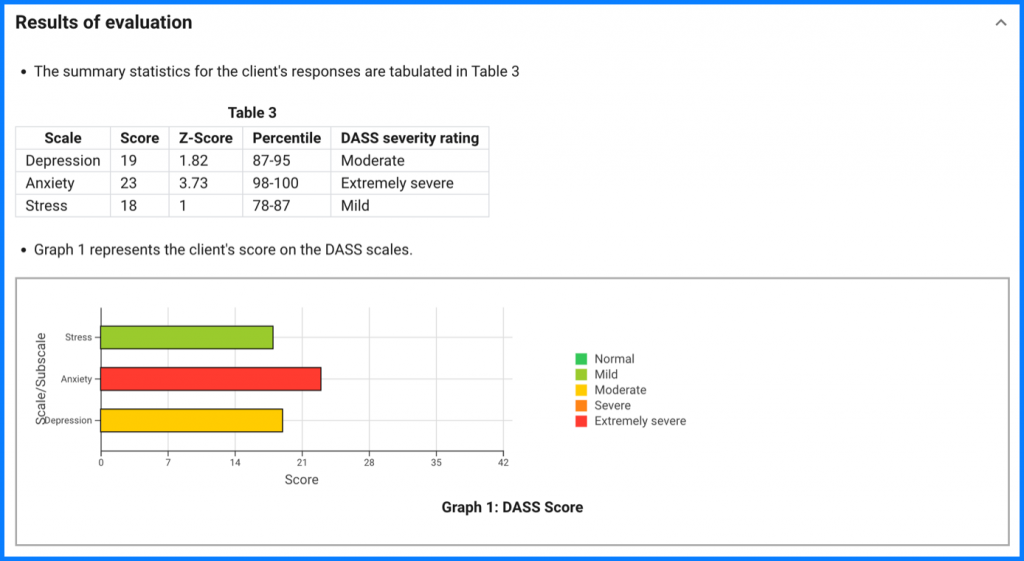
Psychological tests like PHQ-9, GAD-7, IES-R etc. are particularly useful at this stage since they are objective in nature.
Example: The client's results on the Depression, Anxiety and Stress Scale (DASS) signals moderate depression, extremely severe anxiety and mild stress.
It is recommended that you store the data in the client’s file securely in accordance with HIPAA2 . PsyPack is a HIPAA compliant software you can use to conduct psychometric assessments with your clients. It can help you maintain client notes automatically and save you tons of time.
Assessment
This section is the clinician’s analysis of the subjective and objective evidence to arrive at a diagnosis.
For behavioral health practitioners, one would generally expect a differential diagnosis where they would list various problems in order of importance. At this stage, therapists could mention ICD-103 or DSM54 classification of the illness. This can be particularly helpful for therapists who are empanelled and accept insurance plans like United Healthcare5, Aetna6, BlueCross and BlueShield7 etc.
Example: Client is most like suffering from Generalized Anxiety Disorder (ICD-10 code F41.18)
Plan
This section details the treatment approach – interventions, goals/objectives of the intervention, expected time frame, and follow-up and next steps.
Therapists could weigh various psychotherapy approaches like CBT8, EMDR9 etc. at this stage to plan. Additionally referrals to psychiatrists can be considered to pharmacotherapy.
In case, further information is required for planning the treatment, this section will include plan (additional testing, consultation with other clinician etc.) to obtain the required information.
Example: Immediate initiation of pharmacotherapy and, if severe impairment or poor response to therapy, expedited referral to a mental health specialist for psychotherapy and/or collaborative management.
DAP Notes and BIRP Notes
SOAP notes are not the only format available for charting treatment. The other popular approaches include DAP (Data, Assessment, and Plan) and BIRP (Behavior, Intervention, Response, Plan). Among all these formats, SOAP notes format is most widely used.
| Format | SOAP Notes | DAP Notes | BIRP Notes |
| Acronym expansion | • Subjective • Objective • Assessment • Plan | • Data • Assessment • Plan | • Behavior • Intervention • Response • Plan |
| Relationships | • SOAP notes split the Data section of DAP notes into Subjective and Objective elements. • SOAP notes splits the Behavior section of BIRP notes into Subjective, Objective and Assessment sections; and merges the Intervention, Response and Plan elements into the Plan section. | • DAP notes merge the Subjective and Objective elements of a SOAP note under the Data section. • DAP notes splits the Behavior section of BIRP notes into Data and Assessment sections; and merges the Intervention, Response and Plan elements into the Plan section. | • BIRP notes merge the Subjective, Objective and Assessment elements of SOAP notes under Behavior section; and splits the Plan element of SOAP notes into Intervention, Response and Plan elements. • BIRP notes merge the Data and Assessment section of DAP notes under Behavior section; and splits the Plan element of DAP notes into Intervention, Response and Plan elements. |
You should choose the format of documentation based on what’s best suited to your practice. But having a framework can be really helpful. “One of the biggest problems I see with new therapists,” says Dr. Jordan Harris, a professor and trainer in the US, “is a lot of anxiety about how to write adequate professional notes. So many new therapists haven’t been adequately trained and carry a lot of anxiety about having their records audited. Following an official framework, like SOAP notes, can really help relieve that anxiety.” Additionally, you must be wary to not adjust your treatment to fit any particular format. Always remember, treatment notes follow the treatment and not vice versa.
With the advent of AI, idea of using AI-powered note-taking apps to automate progress notes is like a breath of fresh air. Checkout our blog on Streamlining Mental Health Practice: A Guide to AI Note-Taking Apps for Therapists know more.
PsyPack Practitioner’s Notes
At PsyPack, we are constantly working to ensure that therapists are empowered with technology to streamline their practice. Apart from helping you embrace evidence based approach by digitising a wide range of psychological tests, we now allow you to add your own therapy notes to the assessment reports. You can now add notes in any format in the “Practitioner’s notes” section of reports. Try it out.
Today the world is increasingly moving towards mandatorily maintaining treatment documentation. A part of this shift is to ensure best practices, choice of patient to switch their clinician, insurance empanelment and claim settlement etc. To stay competitive, it is critical to embrace best practices and technology in your therapy practice.