A CPT code, or Current Procedural Terminology code, is a standardized code set used in the United States to identify a service or procedure by qualified healthcare professionals. CPT codes were developed and are maintained by the American Medical Association (AMA).
CPT codes are five digit numerical codes and are organized into three main categories:
- Evaluation and Management (E/M): These codes are used to describe services related to patient assessment, examination, medical decision-making, and documentation.
- Procedures: These codes cover both surgical and non-surgical procedures, including diagnostic tests, therapeutic interventions, and other medical services.
- Ancillary Services: These codes encompass laboratory tests, radiology services, pathology services, and other ancillary procedures.
Reimbursement and CPT Codes
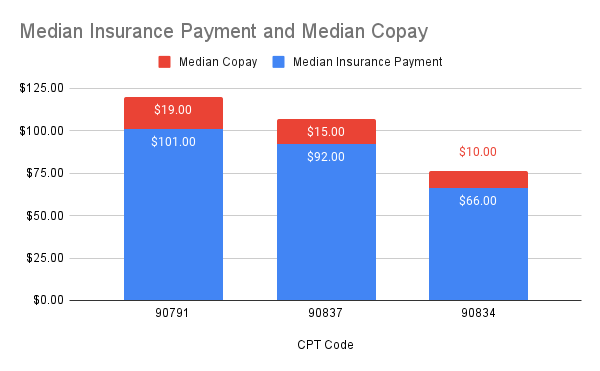
Payments from insurance companies for different CPT codes drastically vary. To understand the earning potential, therapists – particularly the ones running their own private practices, must understand the state of insurance within the mental health industry.
Most used CPT Codes by Therapists
CPT Code 90837 – Psychotherapy, 60 minutes with a patient
CPT code 90837 is used to describe an extended psychotherapy session. Here are some key details about CPT code 90837:
- Code: 90837
- Description: Psychotherapy, 60 minutes with a patient
- Time: The code represents a therapy session lasting approximately 60 minutes.
- Intended Use: CPT code 90837 is used when a mental health professional provides an extended psychotherapy session that goes beyond the typical duration of a standard session, which is usually around 45-50 minutes.
The insurance reimbursement amount for CPT code 90837 may be higher compared to shorter therapy sessions (e.g., 90834 for 45 minutes). It’s important for therapists to meet the necessary criteria and documentation requirements to justify billing for an extended session using CPT code 90837.
CPT Code 90834 – Psychotherapy, 45 minutes with a patient
CPT code 90834 is used to describe a standard psychotherapy session. Here are some important details about CPT code 90834:
- Code: 90834
- Description: Psychotherapy, 45 minutes with a patient
- Time: The code represents a therapy session lasting approximately 45 minutes.
- Intended Use: CPT code 90834 is used when a mental health professional provides a standard duration psychotherapy session that typically lasts around 45-50 minutes.
The insurance reimbursement amount for CPT code 90834 may be different from other therapy session codes, such as shorter sessions (e.g., 90832 for 30 minutes) or extended sessions (e.g., 90837 for 60 minutes).
CPT Code 90791 – Psychiatric diagnostic evaluation, without medical services
CPT code 90791 is used to describe an initial psychiatric diagnostic evaluation. Here are some important details about CPT code 90791:
- Code: 90791
- Description: Psychiatric diagnostic evaluation, without medical services
- Time: The duration of the evaluation is typically 60 minutes or more, but it can vary based on the complexity of the case and the provider’s judgment.
- Intended Use: CPT code 90791 is used to report the initial assessment and evaluation of a patient’s mental health condition by a qualified mental health professional, such as a psychiatrist or psychologist.
The evaluation typically involves a comprehensive psychological assessment of the patient including psychiatric history, current symptoms, social and developmental history, and relevant clinical information. It includes a detailed interview with the patient, potentially involving family members or collateral sources, to gather information necessary for an accurate diagnosis and treatment planning.
Many clinicians often overlook the use of CPT code 90791, which is typically reserved for the initial session with a customer and can only be billed once. Instead, they jump straight to billing 90837 or 90834. This is a common error made by practitioners, causing them to miss out on the advantages and benefits associated with properly utilizing code 90791. The most significant advantage being the reimbursement rate for 90791 which is almost always higher than 90837 and 90834.
Billing 90834 v/s 90837?
Insurance companies typically consider the CPT code 90834 as the standard for outpatient routine care, unless there are unique circumstances involved. Many therapists bill this code for sessions lasting around 50 minutes. However, if the session extends beyond 53 minutes of actual clinical time (excluding scheduling and administrative tasks), the CPT code 90837 is used.
Pushback from insurance companies
If a contracted therapist frequently bills the CPT code 90837, there is a greater likelihood of undergoing a review or audit by the insurance company. This is especially true if the insurance company is providing a higher reimbursement for the 90837 code.
In recent years, insurance companies have raised concerns regarding the use of CPT code 90837. Back in 2015, EquiClaim, acting on behalf of Anthem Blue Cross Blue Shield, sent letters targeting certain clinicians who frequently billed 90837. While the intention of these letters was to provide information, they carried an implication that therapists would need to provide extensive medical records if they continued to use 90837, and could potentially face audits.
Although Anthem Blue Cross Blue Shield apologized for the tone of these letters, providers across the country have received similar communications from Blue Cross and other health plans. These letters inform providers that they are using 90837 more frequently compared to their colleagues and sometimes suggest contacting the Education Team for further discussion.
Tips for billing 90837
Here are key things to keep in mind while billing 90837;
- It must qualify as an hour-long therapy session. The therapy time should be 53 minutes and longer, and not include wait time, scheduling, or documenting.
- Document session start and stop times in the chart.
- Make sure you have a proper justification for using 90837, such as detailed suicide assessment & safety planning, EMDR sessions, ERP sessions, etc.
- You can strengthen the case of billing 90837 if you are using any psychological tests during the session. Using online outcome tools like PsyPack Assessments can greatly assist in such cases as it allows for the generation of comprehensive reports with accurate timestamps.
Underutilized CPT Codes by Therapists
CPT Code 90846 – Family psychotherapy (without the patient present)
CPT code 90846 is used to describe a family psychotherapy session without the patient present. Here are some important details about CPT code 90846:
- Code: 90846
- Description: Family psychotherapy (without the patient present)
- Time: The duration of the family psychotherapy session may vary based on the provider’s judgment and the specific needs of the family. The time range for this code is 26 minutes and above.
- Intended Use: CPT code 90846 is used when a mental health professional conducts a therapeutic session specifically with family members or caregivers, without the patient being present. This type of session focuses on addressing family dynamics, communication patterns, and other issues related to the family system.
Something to be aware of when billing 90846 is that even though the identified client isn’t present, the session still needs to be centered around the identified client’s illness or condition—not the couple or family.
CPT Code 90839
CPT code 90839 is used for appointments that require urgent assessments and examination of the client’s mental state. Here are some important details about CPT code 90839:
- Code: 90839
- Description: Psychotherapy for crisis; first 60 minutes
- Time: 30-74 minutes. The duration of the extended crisis psychotherapy session is specifically 60 minutes. For crisis sessions longer than 74 minutes, a 90840 add-on code (crisis psychotherapy, each additional 30 minutes) may need to be added.
- Intended Use: CPT code 90839 is used when a mental health professional provides an extended psychotherapy session during a crisis situation, typically lasting for the first 60 minutes. This session involves the patient as well as their family members or caregivers to address immediate crisis-related issues and provide support.
Note that the definition of a crisis is really left to the therapist’s clinical judgement. However, examples of this may include clients displaying suicidal behavior or other extreme distress or psychological symptoms where the therapist may need to mobilize resources to reduce potential trauma. Two assessments available on PsyPack Assessments are particularly helpful to screen and assess for self-harm – Ask Suicide-Screening Questions (ASQ) and Columbia-Suicide Severity Rating Scale (C-SSRS). Conducting psychological tests can be helpful in strengthening your documentation and justifying the use of a particular billing code.
Closing notes
As a therapist accepting insurance, it’s a good idea to get empaneled with multiple insurance companies. Using the correct CPT code can make a significant difference in your earnings. You must always be prepared to defend the CPT Code you use. So documentation becomes very important. Using psychological tests can help you build a defensible justification for the use of a particular CPT Code.
Please keep in mind that reimbursement rates and guidelines can differ depending on the insurance company, payer policies, and local regulations. To obtain the most accurate and current information, healthcare providers should refer to the official resources and guidelines provided by the American Medical Association (AMA) and relevant healthcare authorities.