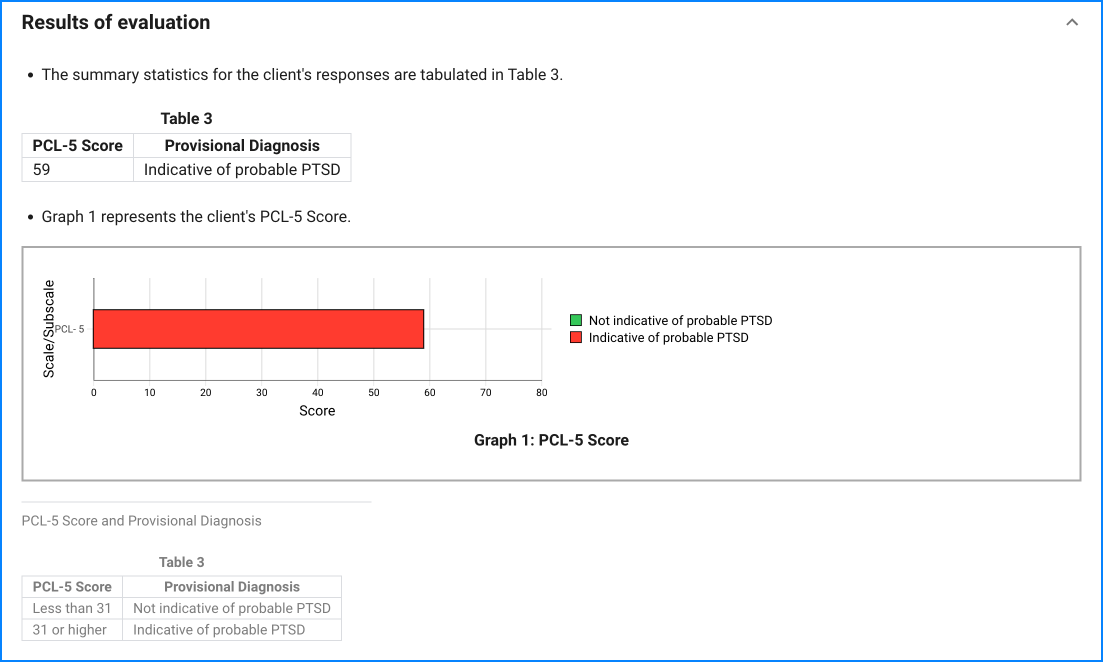
Since the questionnaire relies on client self-report, all responses should be verified by the clinician, and a definitive diagnosis is made on clinical grounds taking into account how well the client understood the questionnaire, as well as other relevant information from the client.
Characteristics of a respondent's setting should be considered when using PCL-5 severity scores to make a provisional diagnosis. The goal of assessment also should be considered. A lower cut-point score should be considered when screening or when it is desirable to maximize detection of possible cases. A higher cut-point score should be considered when attempting to make a provisional diagnosis or to minimize false positives.
The PCL-5 should not be used as a stand-alone diagnostic tool. When considering a diagnosis, the clinician will still need to use clinical interviewing skills, and a recommended structured interview (e.g., Clinician-Administered PTSD Scale for DSM-5, CAPS-5) to determine a diagnosis.
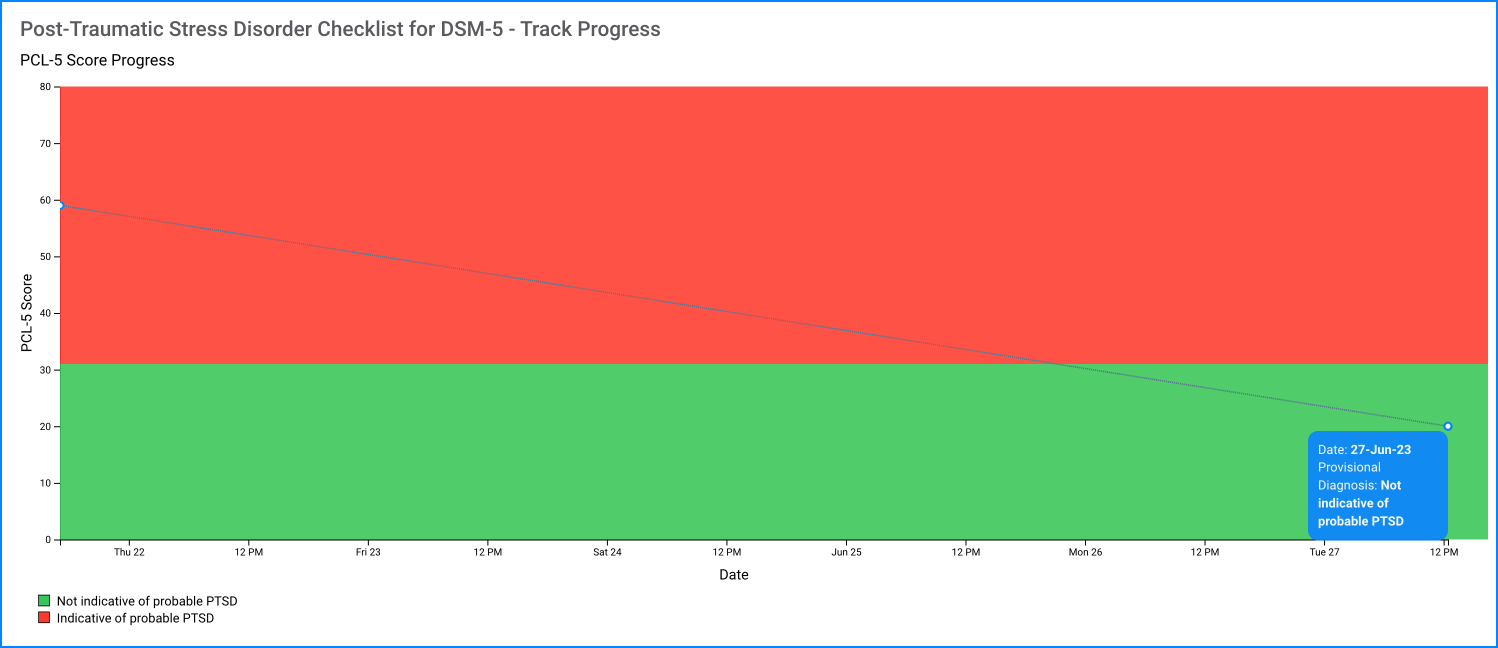
Measuring Change: Good clinical care requires that clinicians monitor patient progress. Evidence for the PCL for DSM-IV suggested 5 points as a minimum threshold for determining whether an individual has responded to treatment and 10 points as a minimum threshold for determining whether the improvement is clinically meaningful. Change scores for the PCL-5 are currently being determined. It is expected that reliable and clinically meaningful change will be in a similar range. We recommend following DSM-IV recommendations until new information is available.