Since the questionnaire relies on client self-report, all responses should be verified by the clinician, and a definitive diagnosis is made on clinical grounds taking into account how well the client understood the questionnaire, as well as other relevant information from the client.
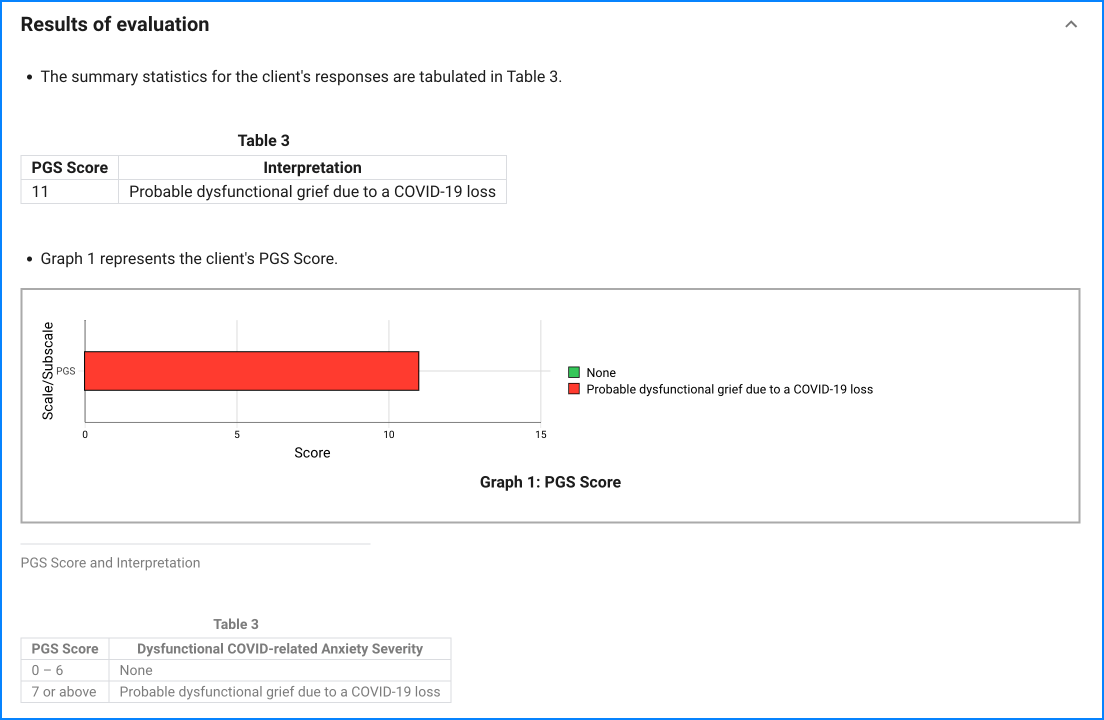
Elevated scores on a particular item or a high total scale score (≥ 7) may indicate problematic symptoms for the individual that might warrant further assessment and/or treatment. Clinical judgement should guide the interpretation of the PGS results.
Endorsement of item 1 (a death wish or suicidal thinking) is an indicator of possible suicidal risk. A final decision about the actual risk of self-harm requires further assessment and clinical interview. Further assessment of suicide risk can be made by asking about the “4 P’s”: past suicide attempts, a plan, probability of completing suicide, and preventive factors.
The PGS holds considerable promise as an efficient and valid measure of problematic grief in the context of bereavement resulting from COVID-19. However, it also could prove valuable in identifying risk of dysfunctional grief resulting from non-COVID losses in the course of the pandemic, as virtually all deaths occurring during this public health crisis are experienced in the same climate of infection-mitigation policies, regulations and general stressors that may adversely affect the mourners’ adaptation, whatever the cause of death.
Psychometric properties: The PGS was developed on a large sample of adults (N = 831) who lost a significant person to COVID-19. The PGS is a reliable instrument (αs > .86), with solid factorial (single-factor), construct (correlates with alcohol/drug coping and suicidal ideation), and incremental (predicts impairment above depression and anxiety) validity. The diagnostic properties of the PGS (87% sensitivity, 71% specificity, and AUC = .87) are comparable to other psychiatric screening instruments, such as the General Health Questionnaire (GHQ).