Scoring System for the EAT-26
Score for questions1-25
Start delivering measurement based mental health care
Conduct psychological assessments remotely, get scores automatically, and maintain clinical records securely
Create account

The Eating Attitudes Test (EAT-26) is a standardized self-report measure of symptoms and concerns characteristic of eating disorders. It is probably the most widely used test used to assess “eating disorder risk” based on attitudes, feelings, and behaviors related to eating and eating disorder symptoms. The EAT-26 is a refinement of the original EAT-40 that was first published in 1979 and used in one of the first studies to examine socio-cultural factors in the development and maintenance of eating disorders.
You can create a free account on PsyPack to access fillable PDFs, manuals and educational resources for the EAT-26©
Scoring System for the EAT-26
Score for questions1-25
Score for question #26
Add the scores for each item together for a total score.
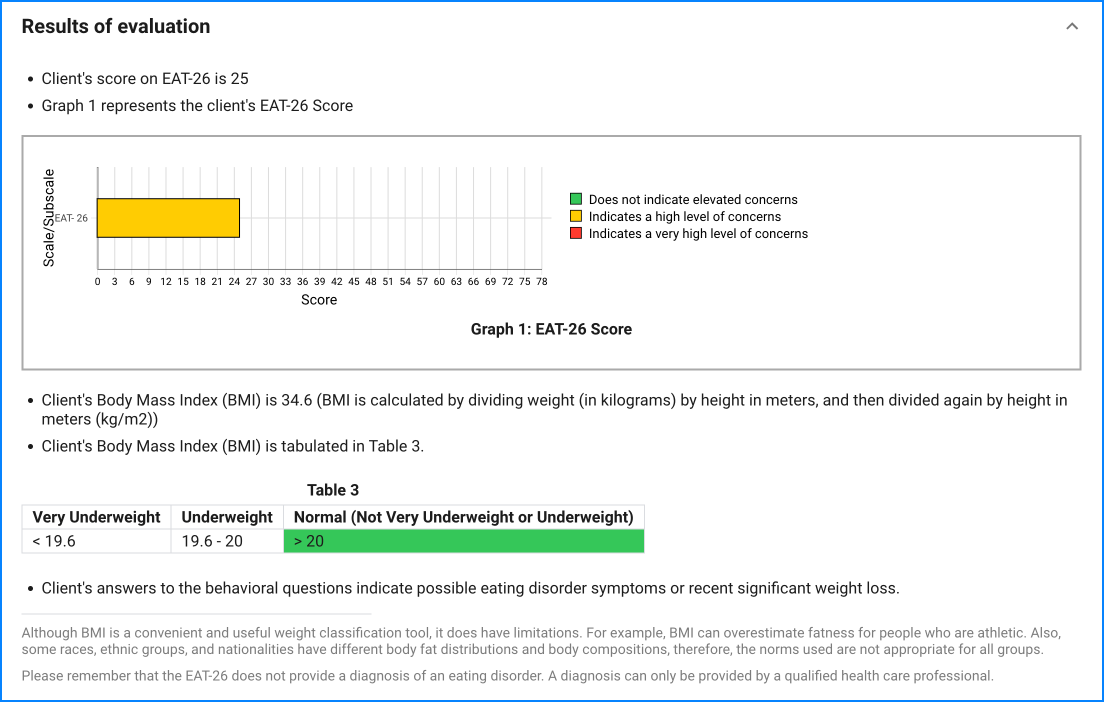
Although BMI is a convenient and useful weight classification tool, it does have limitations. For example, BMI can overestimate fatness for people who are athletic. Also, some races, ethnic groups, and nationalities have different body fat distributions and body compositions, therefore, the norms used are not appropriate for all groups.
Please remember that the EAT-26 does not provide a diagnosis of an eating disorder. A diagnosis can only be provided by a qualified health care professional.
PsyPack can automatically score the EAT-26© assessment and prepare corresponding tables and graphs.
Eating Disorder
The purpose of the evaluation is to:
Self-administered
Clinical
Questionnaire
9 years and above
Less than 5 minutes
Since the questionnaire relies on client self-report, all responses should be verified by the clinician, and a definitive diagnosis is made on clinical grounds taking into account how well the client understood the questionnaire, as well as other relevant information from the client.
Because denial can be a problem on self-report screening instruments, low scores should not be taken to mean that either clinically significant eating disorders symptoms or a formal eating disorder is not present. Collateral information from parents, teammates, and coaches is useful information that can correct for denial, limited self-disclosure, and social desirability. High scores on self-report measures do not necessarily mean the respondent has an eating disorder; however, it does denote concerns regarding body weight, body shape, and eating.
The EAT-26 alone does not yield a specific diagnosis of an eating disorder.
Nevertheless, many studies have used the EAT-26 as an economical first step in a two-stage screening process. According to this methodology, individuals who score 20 or more on the test should be interviewed by a qualified professional to determine if they meet the diagnostic criteria for an eating disorder.
The EAT-26 can be used in group or individual settings and is designed to be self-administered or be administered by health professionals, school counselors, coaches, camp counselors, and others with interest in gathering information to determine if an individual should be referred to a specialist for evaluation for an eating disorder.
The EAT-26 has been particularly useful a screening tool to assess “eating disorder risk” in high school, college and other special risk samples such as athletes (Garner, Rosen and Barry, 1998). Screening for eating disorders is based on the assumption that early identification of an eating disorder can lead to earlier treatment, thereby reducing serious physical and psychological complications or even death.
In addition to the EAT-26 questions, identification of those at risk for eating disorders is based on information on the individual's body mass index (BMI) and behavioral symptoms reflective of an eating disorder. Following the methodology described for the Eating Disorder Inventory Referral Form (EDI-RF; Garner, 2004) four behavioral questions are included on this version of the EAT-26 aimed at determining the presence of extreme weight-control behaviors as well as providing an estimate of their frequency. These questions assess self-reported binge eating, self-induced vomiting, use of laxatives, and treatment for an eating disorder over the preceding 6 months. Although these content areas could be assessed in the same format as other items, this would not provide the type of frequency data required to evaluate the extent of the problem. Body Mass Index (BMI) is also computed and used to determine if the person is“significantly underweight” compared to age-matched norms. Generally a referral is recommended if a respondent scores “positively” on the EAT-26 items or meets the threshold on one or more of the behavioral criteria.
All self-report measures require open and honest responses in order to provide accurate information. The fact that most people provide honest responses means that the EAT-26 usually provides very useful information about the eating symptoms and concerns that are common in eating disorders.
Garner et al. 1982, Psychological Medicine, 12, 871-878